Quality Improvement Tools Pdsa Model
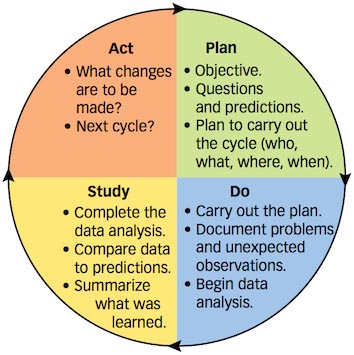

The Plan-Do-Study-Act (PDSA) cycle is part of the Institute for Healthcare Improvement Model for Improvement, a simple yet powerful tool for accelerating quality improvement. Boyz Ii Men Legacy Greatest Hits Collection Rapidshare Library there. Once a team has set an aim, established its membership, and developed measures to determine whether a change leads to an improvement, the next step is to test a change in the real work setting. The PDSA cycle is shorthand for testing a change—by planning it, trying it, observing the results, and acting on what is learned. This is the scientific method, used for action-oriented learning. The steps in the PDSA cycle are: • Step 1: Plan—Plan the test or observation, including a plan for collecting data • Step 2: Do—Try out the test on a small scale • Step 3: Study—Set aside time to analyze the data and study the results • Step 4: Act—Refine the change, based on what was learned from the test The site also includes: • Linking tests of change • Testing multiple changes • Tips for testing changes • Example of a test of change • PDSA worksheet • Project planning form.
Increasing administrative responsibilities—due to regulatory pressures and evolving payment and care delivery models—reduce the amount of time physicians spend delivering direct patient care. A structured approach to quality improvement can help practices successfully implement the change they want to make. Plan-Do-Study-Act (PDSA) cycles provide a straightforward approach to implementing a change in practices and continuing to make improvements. This approach works on many changes from improving a patient care process to executing a new workflow. Plan-Do-Study-Act Release Date: March 2016 End Date: March 2019 Objectives At the end of this activity, participants will be able to: • Select a quality improvement initiative • Implement an improvement initiative • Evaluate the success of the improvement initiative • Adjust the improvement initiative based on the results Target Audience This activity is designed to meet the educational needs of practicing physicians. Statement of Need Engaging practices in quality improvement is “essential to achieving the triple aim of improving the health of the population, enhancing patient experiences and outcomes, and reducing the per capita cost of care, and to improving provider experience.” () Quality improvement initiatives are also essential for setting priorities for areas to improve: if there is no specific plan for measurement, there can be no improvement. This module will guide practices in planning these measurement cycles for true improvements in their practices.
The Plan-Do-Study-Act. Download these ten essential quality improvement tools to help you with your improvement. Whether you use the Model for Improvement.
Statement of Competency This activity is designed to address the following ABMS/ACGME competencies: practice-based learning and improvement, interpersonal and communications skills, professionalism, systems-based practice and also address interdisciplinary teamwork and quality improvement. Accreditation Statement The American Medical Association is accredited by the Accreditation Council for Continuing Medical Education to provide continuing medical education for physicians. Credit Designation Statement The American Medical Association designates this enduring material for a maximum of 0.5 AMA PRA Category 1 Credit™. Physicians should claim only the credit commensurate with the extent of their participation in the activity. Breath Of Fire 2 Gba Deutsch Englisch.
Claiming Your CME Credit To claim AMA PRA Category 1 Credit™, you must 1) view the module content in its entirety, 2) successfully complete the quiz answering 4 out of 5 questions correctly and 3) complete the evaluation. • 1 Plan: develop the initiative Select your improvement initiative Involve your team in selecting the quality improvement initiative. Most good ideas for improvement come from the people doing the work, so consider the perspectives of the clinical team members as well as the clerical staff. Patient surveys can also be used to identify areas for improvement.
To identify areas for improvement, consider asking these questions: • Where does your practice need to improve patient care? • Your practice may already have performance measure data from a or that can reveal gaps in care processes or patient outcomes. • Where is your practice less efficient than it should be? • Staff may be able to identify bottlenecks in the workflow. Prioritize those areas that you have some control over and that the team thinks will be most impactful. Use a “” approach of respectfully observing the work and then asking “why?” A team member can help identify key areas for workflow improvement within the bottleneck.